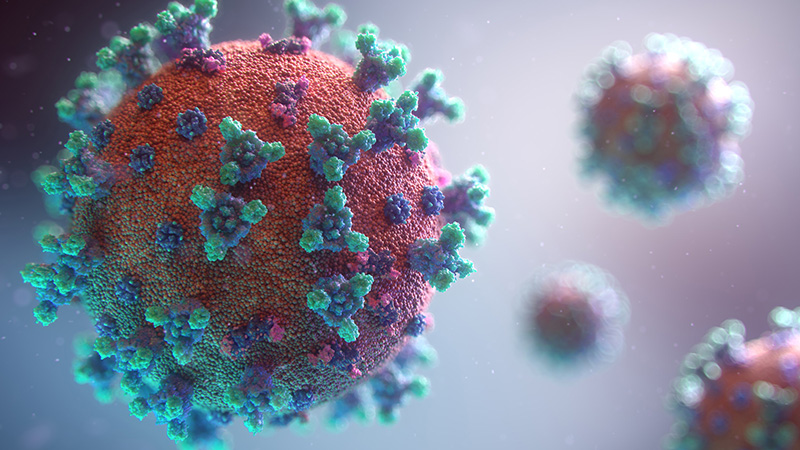
Bad news wrapped in protein
-
Professor Glenda Gray gives insights into the pandemic in South Africa, its impact and its trajectory.
On 19 July, in a much-anticipated webinar, Professor Glenda Gray took alumni on a journey covering the seven-month-old COVID-19 pandemic, which was part historical, part biological and part medical.
Within the first 10 minutes, the webinar reached its 500-person capacity and additional participants were able to view the event live on the alumni YouTube page. https://www.youtube.com/watch?v=crwrVrTKnzw
Professor Gray, a highly respected academic and leader, is the first female President and CEO of the South African Medical Research Council (SAMRC). She is the Chair of the Research Committee on COVID-19, bringing together scientific evidence and experience to the Minister of Health and the National Coronavirus Command Council.
Key early warning system 
She outlined the history of the then “unknown pneumonia”, which could be traced back to 17 November 2019, which morphed into the World Health Organisation’s declaration of a public emergency of international concern on 30 January 2020 which affected 19 countries and had a tally of approximately 7 000 cases.
On 8 January 2020, in the Journal of Travel Medicine, academics who studied travel data and infectious disease vulnerability indices, saw the potential for the international spread of an unknown disease. It listed 20 cities considered to be at risk. Professor Gray emphasised the importance of an early warning system, which must be implemented in future to detect emerging pandemics.
She provided an outline of the four known human coronaviruses, which recur seasonally in two to four year cycles. A major concern is that infection appears to provide immunity from reinfection for only a short period of time. The transmission of COVID-19 is also a concern as it has spread even under lockdown conditions, social distancing and the wearing of masks.
Movement across the globe
Over time the pandemic has moved into low and middle-income settings and continents where testing will be crucial. “The more you test, the more you get a feel of the epidemic, the less you test, the harder it is to understand the burden in your country.” South Africa is currently the only African country which is doing a substantial amount of testing.
The runaway train
South Africa currently has among the highest infection rates in the world. “The reason why our numbers continue to climb is because we haven’t managed to get our infection reproductive rate under zero. The only time you can contain an epidemic is if your reproductive rate is under one. This means one person who has an infection, has not infected one or more people. We’ve always hovered between 1,1 and 1,5. It has had a similar trajectory throughout the lockdown period. By the time we had testing up and running, community transmission had already occurred and we were overwhelmed with testing, with long turnaround times, and were soon unable to identify cases fast enough to isolate their contacts and quarantine them. What happened is the runaway train with community transmission - that’s well established.”
When will South Africa peak?
“We haven’t yet peaked although we are far above the average compared to when European countries peaked...Our trajectory is completely different, (and) similar to what you see in Mexico, Peru and Brazil.”
South Africa seems to be following the trajectory of other low-middle income settings. “We haven’t yet peaked although we are far above the average compared to when European countries peaked.” For example, Gauteng has 33,4 daily new infections per 100,00 population, whereas Italy peaked at 9,3 daily new infections per 100 000 population. South Africa has 19,9 daily new infections per 100,000. “Our trajectory is completely different, (and) similar to what you see in Mexico, Peru and Brazil.”
Bad news wrapped in protein
Professor Gray described the COVID-19 virus as “bad news wrapped in protein”. She said what makes it more severe than other COVID infections is that it invades the deep tissues of the human body, the lungs and the gastrointestinal tract. It is 1000 times better at infecting humans than its closest relative because it evolved from several coronaviruses that merged together. “It is also 1 000 times better at binding to ACE2, which is the called the body’s ‘entry key’.”
The good news
Encouragingly, Professor Gray said there has been a reduction in mortality and ICU admissions in South Africa due to early use of oxygen, high flow nasal oxygen, and the use of dexamethasone and anti-coagulants.
The cumulative cases by age distribution in South Africa as well as hospital admissions mimics global trends. “Most people admitted are 50 years and older. Slightly more men than women are admitted, with very few children admitted or dying. Mortality is associated with comorbidities of diabetes, hypertension, obesity. TB and HIV are also risk factors.
“Children manage the COVID-19 much better. This may be a culmination of them having less ACE2 receptors, a different immune response as well as more recent exposure to other coronaviruses that may provide some cross protection to them. We are trying to see why children are largely spared. But that is good news for all children at a global level.”
Road to a vaccine
Non-pharmaceutical interventions such as wearing masks, social distancing and washing hands remain our main line of defense to prevent its propagation “until the coronavirus circulates out in two or three seasons’ time”. “Normal vaccine development pathways take between 10-15 years. There is a hope that we can get one in 12 to 18 months. But you can see how challenging this is given that it took us 60 years to find a vaccine for polio, 15 for Ebola, and still nothing for MERS (Middle East Respiratory Syndrome) six years later. It’s a very ambitious project and a race against time.”
See more about Wits’ participation in the vaccine search here. /covid19vaccine/


