South Africa has changed tack on tackling Covid: why it makes sense
- Shabir A. Madhi, Fareed Abdullah and Jonny Myers
The South African government has chosen a pragmatic approach that balances the potential direct and detrimental indirect effects of Covid.
In the final days of 2021 the South African government eased its COVID regulations. On December 30th the government scrapped a curfew that had been in place since March 2020. It also initially announced an easing around quarantines and contact tracing but subsequently reversed these plans. Nevertheless, its approach sets a new trend in how countries are choosing to manage the pandemic. Shabir Madhi and colleagues reflects on the boldness – and the risks.
What are the main elements of its new approach?
The South African government has decided to take a more pragmatic approach while keeping an eye on severe COVID and whether or not health systems are imminently under threat. This reflects an acceptance that governments will increasingly be looking for ways to live with the virus cognisant of the detrimental indirect effects that restrictions have been having on the economy, livelihoods and other aspects of society. This is particularly pertinent in resource-constrained countries such as South Africa.
The latest announcements mark a significant departure in the way forward. They mark a pragmatic approach that balances the potential direct and indirect detrimental effects of COVID.
Our hope is that the government continues to pursue this approach and doesn’t blindly follow policies that are not feasible in the local context, and ultimately yield nominal benefit.
The new, more nuanced approach is in stark contrast to reflexively imposing higher levels of restrictions as case rates increased. This suggests that the government has taken note of commentary that has provided suggestions to focus on whether the health facilities are imminently under threat, rather than simply going to higher levels of lockdowns.
The main element of the new approach arises from a high level of population immunity. A sero-survey done in South Africa’s economic hub, Gauteng, just prior to the onset of the Omicron wave indicated that 72% of people had been infected over the course of the first three waves. Sero-positivity was 79% and 93% in COVID-19 unvaccinated and vaccinated people older than 50 years a group that had previously made up a high percentage of hospitalisations and deaths.
The sero-survey data show that immunity against severe Covid in the country has largely evolved through natural infection over the course of the first three waves and prior to the advent of vaccination. This has, however, come at the massive cost of 268, 813 deaths based on excess mortality attributable to 足球竞彩app排名.
The presence of antibodies is a proxy for underlying T-cell immunity which appears to play an important role in reducing the risk of infection progressing to severe COVID. Current evidence indicates that such T cell immunity, which has multiple targets and even more so when induced by natural infection, is relatively unaffected even by the multiple mutations in Omicron and is likely to persist beyond a year. This sort of underpinning T-cell immunity that reduces the risk of severe disease should provide breathing space for at least the next 6-12 months, and possibly beyond that.
Even though Omicron is showing heightened anti-spike protein antibody evasiveness relative to even the Beta variant, vaccine and natural infection induced T-cell immunity has been relatively preserved.
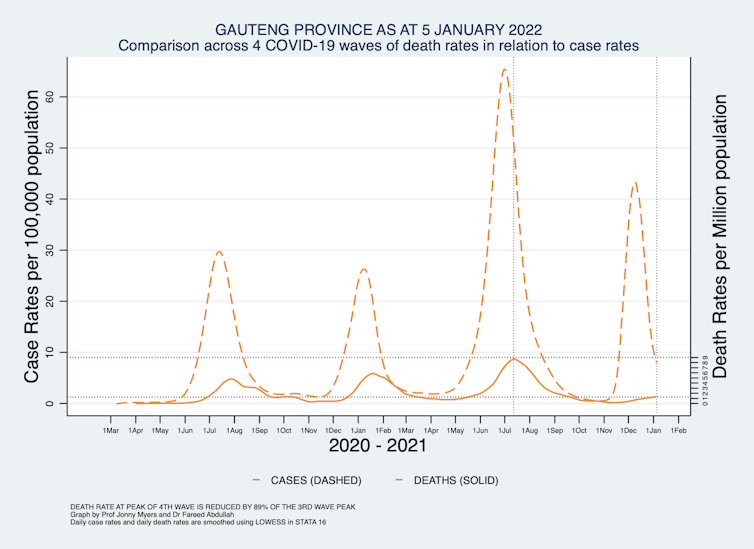
This could explain the uncoupling of the case rate compared with the hospitalisation rate, and even more pronouncedly, with the death rate. In addition, other changing characteristics of the Omicron variant caused by the mutations appear to make it more efficient in infecting and replicating in the upper rather than the lower airway. This could also be contributing to lower likelihood of progressing from infection to severe diseases.
In the meantime it’s crucial that a number of steps are taken.
The drive to ensure higher uptake of vaccines, including booster doses for high-risk groups, needs to continue.
Also, considering that only 10% of infections are actually documented in South Africa because so few people are being tested, a more pragmatic approach to isolation is warranted, mainly if people are symptomatic. This also means that quarantining won’t bring about any major reduction in transmission.
There also needs to be recognition that contact tracing in South African and other similar settings is unlikely to be of any value. This is because the average person in South Africa will possibly have 20 close contacts per day. And even symptomatic infected individuals are most infectious in the pre-symptomatic and early symptomatic phase.
The ineffectiveness of contact tracing and quarantine in limiting the spread of the virus in South Africa is corroborated by three quarters of the population having been infected over the course of the first three waves.
In our view, there is also room for the gradual relaxing of non-pharmacological interventions. In particular, token gesture “hand hygiene” and superficial thermal screening should be scrapped. And there is little reason not to be allowing events such as attendance to outdoor sports events.
Instead, at least for the immediate future, the government should continue focusing on interventions like masking in poorly ventilated indoor spaces and ensuring adequate ventilation.
The issue of mandatory vaccinations is still on the radar, as it extends beyond the added risk that unvaccinated poses to others. And the greater pressure they place on the health systems when they are hospitalised for Covid.
Attention also needs to be given to how incidental COVID infections – people diagnosed with Covid when they’re admitted for a non-related medical issue – are managed in hospitals. The Department of Health guidance needs to be adapted to manage these patients with the appropriate level of skill and resources for the primary reason they were admitted. And patients with severe COVID-19 disease require additional care and expertise to improve their outcomes.
Finally, an evaluation of both vaccination status and underlying immune deficiency needs to become a key element of the workup of hospitalised patients with severe COVID.
Is it clear what the goals are?
The goal has to be minimising hospitalisation and death. It is unnecessary to be stressing out the economy, other health services and livelihoods in South Africa. The death rate with Omicron wave in South Africa is on track to be approximately one-tenth compared to the Delta wave. This means it possibly on a par with deaths caused by seasonal influenza pre-Covid – 10,000 to 11,000 per annum.
This death rate also needs to be considered relative to other preventable deaths. TB is an example, which is estimated to have caused 58,000 deaths in South Africa in 2019.
It’s impossible to say what the characteristics of future variants would be over time. But the experience with the Omicron wave in South Africa provides some comfort that immunity against severe disease and death will continue tracking downward, particularly if vaccine coverage can be increased to 90%, particularly in the >50 year age group. The high force of infection that has likely transpired with Omicron will also further contribute to enhancing protection against severe COVID-19 in the immediate future.
What are the risks?
The major risk is the unpredictability of new variants that evade all aspects of past infection and vaccine-induced immunity. But this is likely to be the result of the evolution of the virus rather than any changes in policy.
Another risk is failure to change the pandemic mindset and failure to appreciate that with Omicron the epidemic phase of COVID-19 is coming to an end. The country and all its institutions and people need to prepare to get back to a previous life – most notably the health services.
The South African government appears to have come to appreciate that the past practices have had limited success in preventing infections, and fully appreciates the detrimental effects that restrictions have had on the economy and society. In addition, it has run out of road to continue with what has unfortunately not yielded much benefit. Despite all the severe lockdowns South Africa still ranks high with a Covid death rate of 481 per 100,000.![]()
Shabir A. Madhi, Dean Faculty of Health Sciences and Professor of Vaccinology at University of the Witwatersrand; and Director of the SAMRC Vaccines and Infectious Diseases Analytics Research Unit, University of the Witwatersrand; Fareed Abdullah, Director: Office of AIDS and TB Research, South African Medical Research Council, and Jonny Myers, Director: Centre for Occupational and Environmental Health, University of Cape Town
This article is republished from The Conversation under a Creative Commons license. Read the original article.

